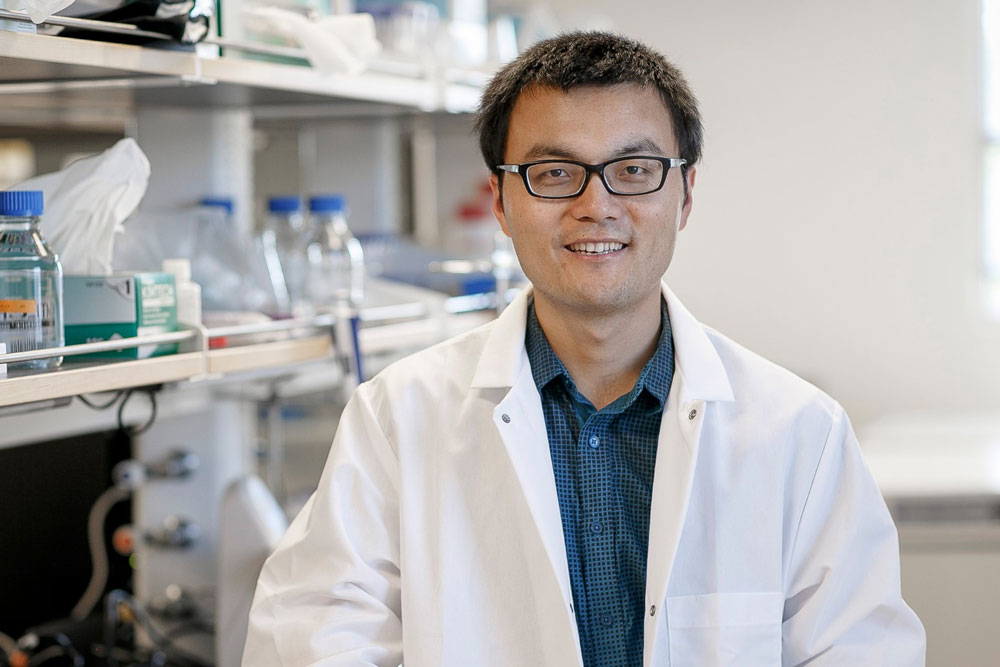
Team Creates Novel Diagnostic Approach for Viruses Using Gold Nanoparticles
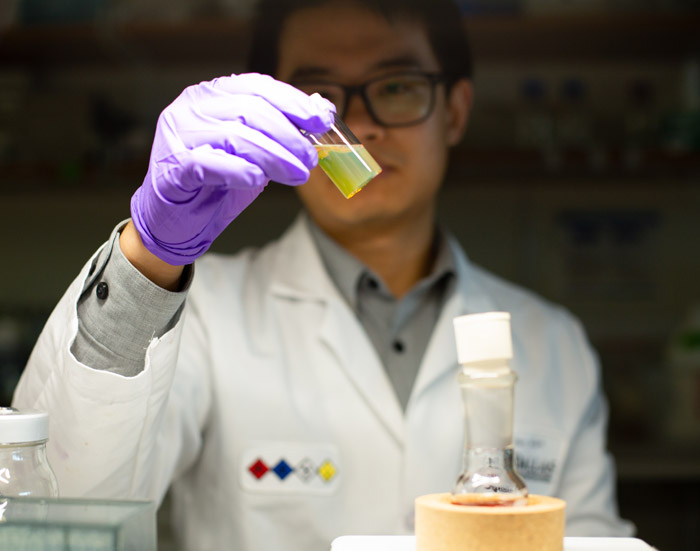
New research from Dr. Zhenpeng Qin, assistant professor of mechanical engineering, was recently highlighted as an important part of the effort to improve rapid testing for infectious diseases including coronavirus.
Researchers at The University of Texas at Dallas have developed a promising method for remotely stimulating activity in deep brain regions, advancing understanding of how molecules act in the brain and paving the way for better cancer treatments and therapies for other diseases.
The approach is based on the powerful combination of gold nanoparticles and lasers, which also plays a critical role in another UT Dallas research project supported by the Congressionally Directed Medical Research Programs and National Institutes of Health aimed at developing a rapid diagnostic test for influenza and, possibly, the COVID-19 virus.
Gold for Neuromodulation
Light is an important tool to modulate biological systems, but absorption and scattering in biological tissues significantly limit its penetration. The system developed by researchers in the Erik Jonsson School of Engineering and Computer Science and the School of Behavioral and Brain Sciences packages molecules inside microscopic gold-coated capsules, or nanovesicles, that can be very sensitive to near-infrared light.
The system could solve challenges in treating diseases, such as ensuring that medication is delivered to difficult-to-reach tumors in deep brain regions while reducing damage to healthy tissue. Using that example, the nanovesicles and their cargo are injected into the brain tissue. External near-infrared lasers that penetrate the tissue cause the capsules to open and release the drug. The researchers describe the approach and results of tests in an animal model in an article published online in the chemistry journal Angewandte Chemie.
“Our system converts light to a mechanical wave that shakes the vesicle open,” said Dr. Zhenpeng Qin, assistant professor of mechanical engineering at UT Dallas and corresponding author of the study.
Other researchers have used near-infrared light to trigger drug-carrying nanoparticles, such as phospholipid liposomes, which release their cargo when heated by the laser, but Qin’s approach with gold-coated nanovesicles uses about 40 times less laser energy.
In tests in animal models, Qin and his colleagues found that the near-infrared light penetrated 4 millimeters in the brain, which was enough to reach most targeted brain regions. Qin said he anticipates the laser penetrates far enough to reach targets deep in the rodent brain that will help answer important questions in neuromodulation.
While the nanovesicle system must undergo more development and testing before it could be used in clinical care, Qin said the approach eventually could be applied to neurological disorders or other cancers. Dr. Hejian Xiong, research associate in Qin’s lab and co-author of the journal article, received a new postdoctoral fellowship from the Phospholipid Research Center in Germany to study the use of gold-coated nanovesicles and ultra-short near-infrared lasers to target and relieve pain in patients after surgery. The project aims to provide an adjustable pain management system that could reduce the need for opioids.
Millions in Federal Funds Support Infectious Disease Testing
In separate research work, Qin recently received nearly $2.8 million to develop a rapid, accurate and less expensive test for infectious diseases, including influenza, that could be conducted in doctors’ offices. The testing principle could also be applied to diagnose COVID-19. The Congressionally Directed Medical Research Programs awarded $293,000, and the National Institutes of Health awarded $2.5 million over five years.
The grants support efforts to advance the gold nanoparticle approach, develop prototypes and evaluate the method using clinical specimens, Qin said.
While many doctors conduct rapid flu tests on site, the tests can miss influenza in 30% to 50% of cases, according to the Centers for Disease Control and Prevention. Samples must be sent to a lab for an accurate diagnosis, which can take days.
“We want to improve the tests’ sensitivity so that doctors can make the judgment call right in front of the patient, to be able to say either you have it or you don’t have it,” Qin said.
In the testing method, gold nanoparticles are attached to antibody molecules that can recognize and bind with protein molecules found on the surfaces of viruses. Researchers apply short laser pulses to activate the nanoparticles to generate nanoscale bubbles, or nanobubbles. The accumulation of the nanobubbles signals the presence of a virus.
“By using optics to detect and count the nanobubbles, we can sensitively and quickly detect the presence of specific respiratory viruses,” Qin said.
One of the advantages of the approach is that it would not require extensive sample preparation, Qin said. The method could help doctors diagnose viruses much faster and reduce health care costs by eliminating the need for expensive lab visits. The approach could be used to detect a single virus or multiple viruses.
Ultimately, researchers envision the test being broadly used in hospitals and clinics that do not have labs; however, the diagnostic method will need to be tested further before it can be made widely available.
Qin’s group is not working with the live coronavirus, only with viral genes, proteins and antibodies. Qin has previously obtained such patient samples for his research on respiratory syncytial virus and influenza. The NIH Grant (1R01AI151374) is focused on RSV, but Qin said the diagnostic method can be applied to detect other viruses.
An Interdisciplinary Collaboration
Other UT Dallas authors of the Angewandte Chemie study from the Department of Mechanical Engineering are co-first authors Xiong and Dr. Xiuying Li, research scientist, as well as Peiyuan Kang, a PhD student. Other contributors include researchers from the School of Behavioral and Brain Sciences: Dr. Jonathan Ploski, associate professor; Dr. Sven Kroener, associate professor; and John Perish, a cognition and neuroscience PhD student.
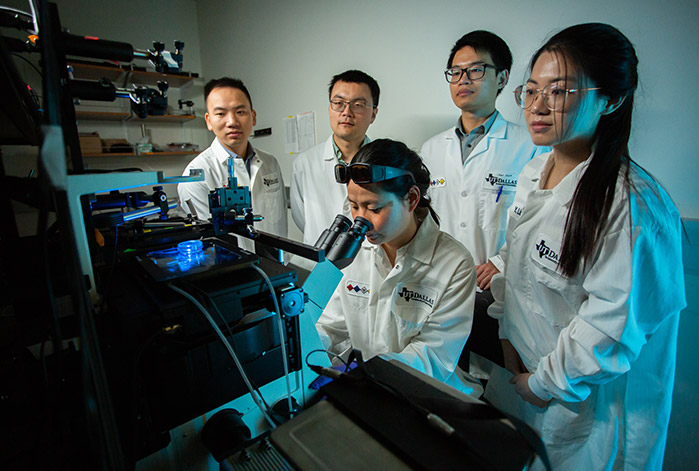
Researchers from the Swiss National Centre of Competence in Research in Chemical Biology, University of Minnesota, Athinoula A. Martinos Center for Biomedical Imaging at Massachusetts General Hospital/Harvard Medical School, Icahn School of Medicine at Mount Sinai, and Acthera Therapeutics in Switzerland also contributed.
The research was supported by The University of Texas System Neuroscience and Neurotechnology Research Institute, the National Science Foundation, National Institute of Neurological Disorders and Stroke (grant number RF1NS110499) and the Swiss National Science Foundation.
Media Spotlight: COVID-19 Response

Posts
You May Also Like